Tiny Maria Perez stretches out in her neonatal intensive care (NICU) incubator, arms overhead, as if she’s enjoying her massage and breathing therapy. Born 17 weeks too early and weighing only 1.18 lbs. on Aug. 18 at Community Regional Medical Center, Maria gets an innovative treatment that uses percussive bursts of air to open up her lungs’ tiny air sacs and helps keep her off a ventilator.
And every three hours a NICU nurse and a respiratory therapist at Community Regional team up to change Maria’s respiratory apparatus from a mask to nasal prongs. This ensures that her fragile skin isn’t rubbed raw. When the skin degrades, very premature infants have to be put back on a more invasive ventilator.
The every three-hour respiratory routine is a simple idea that makes a huge difference for these tiniest babies – for the rest of their lives.
Because preemies at Community Regional are able to stay off ventilators, only two out of the 857 babies in its NICU last year went home needing to use oxygen. Statewide nearly 10% of very premature babies cared for in similar NICUs get discharged with oxygen tanks, according to the California Perinatal Quality Care Collaborative. And while oxygen is necessary for those struggling to breathe, it can be corrosive to tiny lungs over time and can cause visual problems, explained Hank Perry, clinical coordinator of respiratory care at Community Regional’s NICU.
Fresno County’s premature birth rate of 10% is among the highest in California, rivalling some third world countries and Community Regional ranks second in California for delivering the most babies weighing under 3 lbs. 5 oz. As the high-risk pregnancy and delivery center for a 5-county area, about 15% of the babies born at Community Regional are cared for in the NICU. Because of their long experience with the tiniest babies, Community NICU physicians and staff have developed a number of best practices to help under-developed lungs function better.
Perry shared the practices Community Regional uses to help premature babies breathe better with a national audience at the Dec. 4 “Hot Topics in Neonatology 2016” symposium in Washington D.C. He was the only non-physician presenter among leading experts in neonatal respiratory care.
Community Regional delivers lung surfactant, a critical medication, to babies born at 22-29 weeks gestation, faster than any other hospital in the state since respiratory care practitioners, pharmacists and neonatologists are part of the delivery team during high-risk and premature births. More than 82% of Community Regional’s extremely low-weight babies get this crucial lung treatment within the first 30 minutes of birth – nearly twice as fast as the statewide average.
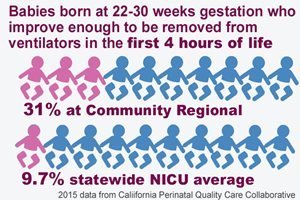
And preemies at Community Regional are three times more likely to improve enough within the first four hours of life to be taken off a ventilator, compared to premature newborns at NICUs statewide. More than 31% of Community Regional babies born 11-18 weeks early spend less than four hours on a ventilator and 67% of those extremely premature babies improve enough be removed from the ventilator within their first 24 hours of life. By comparison, the average ventilator removal rate among babies in the 131 California NICUs tracked by the Quality Care Collaborative is 9.7% during the first four hours and 48% within the first 24 hours.
“We put babies on ventilators right after birth much more than other hospitals, but we get them off much faster than anyone else,” said Perry. “The quicker you can remove these infants from the ventilator the better to reduce damage to the lungs that causes chronic lung disease.” Because of these practices premature babies are less likely to have asthma later in life, Perry added.
|
|
|
Community Regional is ranked #2 in California for delivering the most babies weighing under 3 lbs. 5 oz |
|
|
|
3x more extremely premature babies at Community Regional improve enough in the first four hours of life to be removed from ventilators compared to NICUs statewide |
Another technique Community Regional uses to help babies breathe easier is an intrapulmonary percussive ventilator (IPV), which uses small percussive bursts of air to loosen and free mucus from airway walls and to open the lungs’ tiny air sacs. Perry said, while IPV is used frequently for adults, especially those with cystic fibrosis, it is rarely used in tiny newborns. But after finding it was a common practice in Europe with great results for preemies, Perry worked to get the practice introduced at Community Regional.
The every-three-hour respiratory change is also a best practice. It takes a team effort to change the bubble CPAP (continuous positive airway pressure) from mask to nasal prongs. NICU nurses and respiratory therapists gently massage their tiny patients’ heads compressed in tight-fitting caps that help hold the CPAP in place. Medications are delivered and feeding tubes are checked and diapers changed all at the same time. “We do everything together. It’s called cluster care,” Perry explained. “So the baby can be left to eat, sleep and grow in the three hours in between each change.”
Studies show that long periods of leaving premature babies alone with minimal stimulation better simulates being in the womb and improves preemie’s brain development. IPV and the other treatments are helping Maria’s lungs grow stronger every day, said her mother Yesica Perez.
“These are simple practices that should be standard practices but not a lot of hospitals are doing this,” Perry said. “It makes a big difference.”
Erin Kennedy reported this story. She can be reached at MedWatchToday@communitymedical.org


_138.jpg)