Peggy Grant, PhD, Director of Innovation and Performance Improvement at Community Regional, has been invited to share the hospital’s experiences equipping nurses with bedside tools to educate patients at the HIMSS16 (Healthcare Information and Management Systems Society) conference in Las Vegas in March. Peggy answered questions about the innovative practices Community Regional pioneered and will present on the national stage. [See preview coverage of Peggy’s talk in HealthIT online.]
 Q. What will HIMSS16 conference attendees learn from your session?
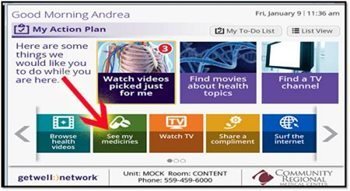
Q. What will HIMSS16 conference attendees learn from your session?Peggy Grant: My session “Hardwiring Technology into Care Delivery to Increase HCAHPS” outlines how Community Regional utilized the excellent integration work developed through the collaboration of Community nurses and Epic electronic medical record system builders with GetWellNetwork. This integration resulted in streamlining the delivery and documentation of medication teaching for nurses and pharmacists at patients’ bedsides, as well as detailing other methods and tools for increasing patient satisfaction and increasing HCAHPS scores. I’ll share how we’re using technology to ensure that patient education is part of the nursing day and how technology helps us be more efficient.
Q. How big a difference is this clinical process and IT integration making?
Peggy Grant: Community Regional began integrating GetWellNetwork, an interactive patient care software and video delivery system, with our Epic electronic health record system and other health IT technologies in 2013 to improve clinical workflows and to document medication teaching. Some units, using the interactive patient care system, saw significant improvements in their HCAHPS scores.
We looked at fiscal year 2015 and compared it to a baseline in April through June of 2013 to check whether patients reported on the HCAHPS surveys that the hospital staff explained the side effects of their medications in a way they understood, that staff told them what the medicine they were taking was for and that they were communicated to well about their medications.
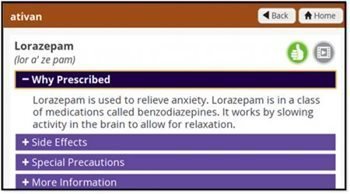 Overall, Community Regional’s score in medication communication increased by 5%. When we took a deeper look at four specific units, we saw an average increase of 14.4% in HCAHPS scores on those three measures with the most dramatic increases in patient’s understanding about what their medication was for and feeling like staff communicated well to them on that issue. In one unit that HCAHPS score went from an average of 62.5% patients answering yes to 92.2% answering yes.
Overall, Community Regional’s score in medication communication increased by 5%. When we took a deeper look at four specific units, we saw an average increase of 14.4% in HCAHPS scores on those three measures with the most dramatic increases in patient’s understanding about what their medication was for and feeling like staff communicated well to them on that issue. In one unit that HCAHPS score went from an average of 62.5% patients answering yes to 92.2% answering yes.What’s more, the impact of the initiative has gone beyond the HCAHPS scores themselves and has really impacted clinical practice. We’re leveraging technology to train staff, educate patients and measure results.
Q. What else is this kind of technological integration helping?
Peggy Grant: We’ve been able to get data from our EHR, such as how many videos are ordered by staff, and the percentage of videos ordered by staff compared to length of stay. So unit managers can look at that data and know how much education their patients are getting and correlate that to outcomes.
Q. What was key to making the improvements and fully integrating technology in the nursing practice?
Peggy Grant: We have great technology and software systems, but what really helped was having strong leadership engagement and a solid education plan to get buy-in from our nursing staff. We’re constantly working on that.
We know now that consistent, effective patient education is a learned skill that requires standardized clinical education. Additionally, the use of regular feedback to nurses gleaned from looking at the metrics provided by our technology, reinforces their accountability and really makes it part of the patient care routine. The GetWellNetwork’s interactive education needs follow up and reinforcement by the bedside nurse.
Q. Why is this model of patient care crucial in today’s healthcare?
Peggy Grant: Engaging patients is really required to help transform hospital care. As payment models move from a fee for service model to paying based on keeping patients healthy, on the quality of the care and the patient’s perception of their care our clinicians need to shift from being providers to partners in healthcare. Using interactive patient care education helps engage patients as partners in their healing and care.


